Written by: Robert L. Bard, MD | Lennard M. Gettz, Ed.D | Noelle Cutter, PhD | Josh T. Schueller, PT
MEDTECH SPOTLIGHT: TCD FROM RADIOLOGY TO VASCULAR STUDIES
From an interview with Maty Torres, BHSc, RVT
In our ongoing study of non-invasive diagnostic modalities, we connected with Chief Vascular Technologist & Technical Director of Cooperman Barnabas Medical Center's (CBMC) Non-Invasive Vascular Lab, Ms. Maty Torres. Her vast experience on the use of the Transcranial Doppler provided extensive insight on its many advantages in patient care for both Radiology and Vascular units.
As a career technologist, Ms. Torres started in vascular sonography (1990) then received her first exposure to the field of TCD scanning 1998. In the early part of her tenure, she performed Transcranial Doppler Imaging on a patient population from the Valerie Fund Children’s Center (A NJ based non-profit group providing support for the comprehensive health care of children with Cancer and blood disorders) for pediatric sickle cell patients. By 2011 her expertise with cerebral doppler scanning were called to new challenges.
As a team-supporting service, Ms. Torres advanced to the next stage of TCD utility in non-imaging TCD exam where this protocol provided great data-gathering advantages in emergent and post-surgical cases for medical collaboration between residents and neuro specialists by monitoring subarachnoid hemorrhage patients for new onsets of vasospasm in Neuro ICU cases. She expresses the major LEARNING CURVE behind being proficient at operating TCD scanning. "This is not a test that you could cross train in a short period and perform it adequately. Without an image for guidance, you are using audible sounds, waveforms, and direction of flow, thus relying on the technologist’s expertise to find the correct arteries. I have seasoned technologists that range from 11 to 20 years of experience in the field; however, only few perform this study because it’s very specific.”
Ms. Torres adds, “When a patient is admitted with a subarachnoid hemorrhage, the goal is to search for the source. Some patients might require Endovascular Coiling (treatment to block blood flow/bleeding throughout the body) and recover in the Neuro ICU. We support the neuro team by providing scheduled monitoring by daily TCD’s evaluating increases in ratios that could detect an increased risk of an onset of vasospasm."Her facility currently uses the Nicolet® SONARA® TCD system. While these hospital-grade devices can be used for Emboli detection or interoperate scanning for PFO (Patent Foramen Ovale) closures, Ms. Torres' current assignments are primarily focused on neuro-monitoring for the detection of increased risks of vasospasms. As a seasoned technical expert in various levels of TCD field use, Ms. Torres shares field insight on the medical applications of this diagnostic protocol. "I see an opportunity to use TCD for patients with symptomatic carotid stenosis at our facility.”
SPECIAL TRAINING
Her training on TCD imaging first started in 2001 with an intensive training course presented by Medical College of Georgia School of Medicine led by Dr. Robert J. Adams currently at the Medical University of South Carolina working directly on Sickle Cell patients. Dr. Adams is considered a pioneer in using transcranial doppler (TCD) and transcranial Doppler imaging (TCDi) to assess stroke risk in children with sickle cell anemia (SCA). He also helped discover that regular blood transfusions can reduce strokes by as much as 90 percent in these children.[4] Additional training came from Natus training experts who come from many areas such as the Swedish Institute of Neurology and a comprehensive text: Practical Guide to Transcranial Doppler Examinations by Dr. Andrei Alexandrov.
PART 2: VERIFYING SIGNS OF COVID-19 STROKE THROUGH IMAGING
By: Robert L. Bard, MD and Dr. Pierre Kory, MD
We have learned over the last century that blockages of coronary arteries to the heart and carotid arteries to the brain are precipitated by inflammation of the inner walls of the vessel, called the “intima”
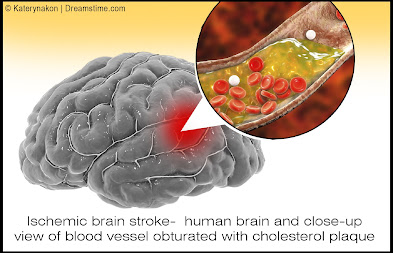
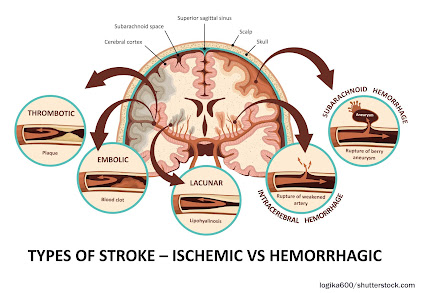
While thickening of the interior wall of vessels gradually occurs over time and is aggravated by diet, stress and hypertension (high blood pressure), the acutely disabling event occurs when there is an abrupt tear of the overlying plaque which ruptures debris which then forms a blood clot which blocks blood flow or the clot travels deeper into the brain and blocks blood flow. Similarly, abnormal heart rhythms such as “atrial fibrillation”, causes the pooling of blood in the heart which predisposes to clot formation and the clots can then travel into the brain causing a stroke. In Covid-19, the virus causing severe inflammation in the blood which then promotes clot formation which can travel through the vascular system and affect almost every organ system in the human body, with the brain and lungs being the most vulnerable. An article in September NEUROLOGY reported by Medscape documented the incidence of large artery stroke as the presenting symptom of COVId-19 was highest in men under the age of 50 years. [4]
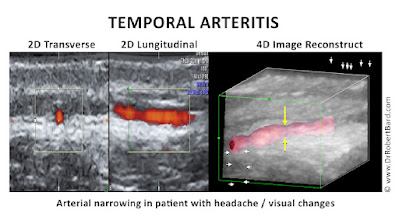
However, the chronic and diffuse nature of arteritis often weakened the vessel wall producing aneurysmal dilation and rupture. Today we find sophisticated non-invasive or minimally invasive modalities to be the first line of interrogation of vasculitis. [5]
| - Carotid Sonogram - Carotid Doppler - Eye Sonography - Transorbital Doppler - Contrast Enhanced Ultrasound - Transcranial Doppler - Hybrid Imaging |
- 3D/4D Vessel Density Histogram - Endoarterial 3D Doppler - Retinal OCT - Soft Tissue OCT - Reflectance Confocal Microscopy - Small Coil MRI - 7 Tesla MRI |
CAROTID SONOGRAM: While cerebrovascular disease is often diagnosed ex post facto after a catastrophic episode with MRI and CT, the non invasive Doppler analysis of the vascularity is generally checked with ultrasound for plaque and obstruction. A useful measure of the risk of coronary and cerebrovascular disorder is the carotid intimal thickness (CIMT). Standard depth of the inner wall thickness is a measure best obtained by high resolution sonograms since a reading over 0.9mm indicates increased risk. The newer sonogram units have depth resolution of 0.02mm making this a preferred non invasive option.
DOPPLER IMAGING TECHNOLOGIES - COLOR DOPPLER - most common application where red is flow towards the probe and blue is flow away from the probe - POWER DOPPLER - higher spatial resolution without directional flow correlation - 3D POWER DOPPLER - allows volumetric analysis of vessel density used in treatment correlation where more vessels means increased neovascularity and fewer vessels correlates with clinical improvement - ANGIODOPPLER – similar to color Doppler with higher spatial resolution - MICROVASCULAR DOPPLER-images capillary flow - B-FLOW DOPPLER-not true flow technology but observes motion of red blood cells directly CAROTID DOPPLER: Flow abnormalities of turbulence and absence are commonly evaluated with this modality. Plaque forms more readily in aberrant flow patterns and high velocity regions accompanying narrowing. EYE SONOGRAPHY: Sonofluoroscopy of the orbital soft tissues and eyes is performed in multiple scan planes with varying transducer configurations and frequencies. Power and color Doppler use angle 0 and PRF at 0.9 at optic nerve head. 3D imaging of optic nerve and carotid, central retinal arteries and superficial posterior ciliary arteries performed in erect position before and after verbal communication. Retinal arterial flow is measured. Optic nerve head bulging is checked as increased intracranial pressure may be demonstrable. TRANSORBITAL DOPPLER: R/L ciliary arteries have normal Doppler flows of 10cm/s which is symmetric. CONTRAST ENHANCED ULTRASOUND: Widely used European nonionic contrast injection allows imaging capillary size vessels and perfusion characteristics TRANSCRANIAL DOPPLER: This measures the flow in the anterior, middle and posterior cerebral arteries as well as Circle of Willis. 3D/4D VESSEL DENSITY HISTOGRAM: Multiple image restoration and reconstruction shows retinal vessel density of 25% at the optic nerve head and adjacent region with quantitative accuracy.[8] ENDOARTERIAL 3D DOPPLER: Microcatheters inserted into the arterial or venous system provide measurement of wall thickness and presence of inflammatory vessels inside the intima. RETINAL OCT: Subtraction techniques done with OCT optical coherence tomography may show changes in the caliber of the retinal vessels with verbal ideation. SOFT TISSUE OCT: The depth of penetration may be extended to 2-3mm allowing for analysis of vascular changes in erythematous or erythropoor dermal areas. Thrombosis may be observed. REFLECTANCE CONFOCAL MICROSCOPY: This microscopic analysis of the cells also quantifies microvascular pathology and is a potential modality for studying vasculitis. SMALL COIL MRI: High resolution systems used for animal study and superficial organs can image the intra-arterial anatomy including dynamic contrast imaging on standard 1.5T and 3T units. 7 TESLA MRI: High field systems analyze signal abnormalites rapidly with high resolution. HYBRID IMAGING: Hybrid imaging refers to combining diagnostic modalities to assess disease and monitor therapy. |
Disclaimer: The information (including, but not limited to text, graphics, images and other material) contained in this article is for informational purposes only. No material on this site is intended to be a substitute for professional medical advice or scientific claims. Furthermore, any/all contributors (both medical and non-medical) featured in this article are presenting only ANECDOTAL findings pertaining to the effects and performance of the products/technologies being reviewed - and are not offering clinical data or medical recommendations in any way. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, never disregard professional medical advice or delay in seeking it because of something you read on this page, article, blog or website.
REFERENCES
1) Hemodynamics: https://en.wikipedia.org/wiki/Hemodynamics
2) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5224659/
3). Hassani SN, Bard RL: Ultrasonic Diagnosis of Aortic Aneurysms. J. Natl. Med. Assoc. 66:298-299, July 1974
4). Lande A, Bard RL: Arteriography of Pedunculated Splenic Cysts. Angiology 25:617-621, October 1974
5). Lande A, Bard RL, Rossi P: Takayasu's Arteritis: A World Entity. N.Y. State J. Med. 76:1477-1482, Sep 1976
6). Helbick Eur Radiol 30:5536-5538, 2020
7). Mao l JAMA Neurol 2020 77:683-690
8). Bard RL , Gettz L, van der Bent S etal: Proceedings of the 4th Inflammatory Disease Summit at NY Academy of Medicine Nov 2021