Interview by: Lennard Gettz, Ed.D & Roberta Kline, MD
Edited by: Dr. Robert L. Bard
Introduction
In support of personal leadership and proactive health, The Integrative Pain Healers Alliance applauds Ms. Suzanne Wheeler of Minneapolis, Minnesota as our Researcher of the Month. After years of suffering a life-altering disorder that currently continues to challenge the scientific community of its root causes, Suzanne explored “outside the conventional box” of opioid prescriptions until she uncovered the one remarkable solution that got her back on her feet and joining life again. Invoking CHANGE against all odds by diligently searching for what’s beyond the convenient takes courage and conviction. It is this level of leadership that defines Alternative Health and Wellness to educate others about new answers that offer better results.
SHOT DOWN BY CFS
In 2017, I was diagnosed with Myalgic Encephalitis or Chronic Fatigue Syndrome. I had been essentially home bound for about two years and probably bed bound about 50% of my time. CFS was found to be the source of my 'all over body' pain- and so started my road to seeking out more targeted treatments.
Life before CFS was very active. I worked in corporate America for 17 years as a regional manager for a large building facilities company and managed a team of about 3000 people. Prior to that, I was in the United States army for a decade. I was a Blackhawk pilot and a C 12 airplane pilot in the military before I entered corporate America.
I started to feel significant pain after the birth of my 3rd daughter in Oct 2002. I had a traumatic delivery due to a condition called placenta previa. I lost over half my blood volume during the birth and received extensive blood transfusions. I never felt the same after that experience. About a week after delivery, the pain throughout my body started. Over the years – it became worse and worse, and the fatigue became debilitating. I kept pushing through with my job and family responsibilities which may have damaged my body even further.
CFS is not an easy problem to resolve. I spent extensive time at Stanford University's chronic fatigue clinic with some of their top specialists. I was also sent to the Workwell Foundation (CA) where I underwent a two day CPET (image insert) a cardiopulmonary exercise testing where they were able to determine what my anaerobic threshold was my VO2 max. It was there that the clinicians found the extent of my metabolic dysfunction; my reports showed a VO2 reading equivalent to that of about a 95 year old.
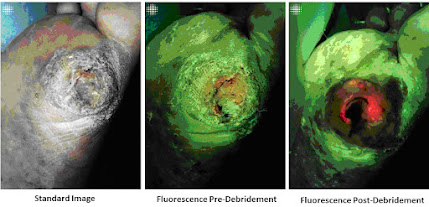
I had the kind of pain that radiated all over- throughout my spine, throughout my hips, legs, my knees, ankles, feet also throughout my arms. I had, peripheral neuropathy in my hands. I had trouble moving my hands and trouble typing and then also trouble walking. It developed to the point where in 2015 I was using a cane in my late forties to walk. I was desperate to get pain relief for more than a decade. I also had compression in my lower spine and my L4, L5, and also in my thoracic region (T 11 & 12) that caused extensive pain. It wasn't an easy thing to figure out but through MRI, you can see the physical deformities- where imaging helped make everything pretty clear. But as to why it radiated through my body like it did, it took a lot of years to find out.
DESPERATE FOR PAIN RELIEFSince 2002, I tried everything- modalities from opioids to hip injections to spinal injections from a pain clinic. I saw chiropractors, I had acupuncture, tens units, electrical stim, laser treatments, extensive cranial psychotherapy, massage, a lot of ice and heat, a massage chair and a hot water Jacuzzi (which was the one thing that I responded to the best).
All pain relief from this point was temporary. The base pain would eventually return and continue to get progressively worse. Years into this, it didn't seem like there was a lot left for me to try. I learned that my condition was based on a specific virus that destroys your metabolic system and your body doesn't have the ability to oxygenate for energy. I was extremely tired all the time with post exertional malaise and my anaerobic thresholds became very low. Our body builds up lactic acid with any exertion, with even minimal amounts of exertion.
TAKING CHARGE: RESEARCH OUTSIDE THE BOX
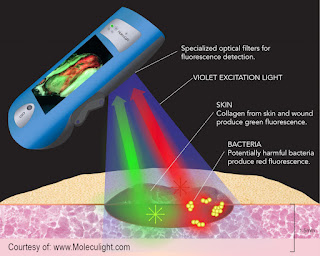
In 2017, I learned about PEMF and its concepts of getting to the cellular level by helping my cells oxygenate. Reading the many testimonials about it, it seemed to make better sense than the other modalities I tried so far. User stories matched up with my symptoms and what I had been told by doctors was happening to my body. My sister introduced me to the idea upon seeing a presentation at a horse event, believe it or not. I became intrigued and acquired a rental and eventually purchased my own model.
ALTERNATIVE HEALTH
I have HAD some wonderful physicians who are experts in their lane. At the height of my illness, I was seeing six different doctors who had me on so many medications (10 or 12 prescriptions) and I was still bed ridden- hence, nothing was working.
Before I started using the PEMF, I had been essentially home bound for about two years and probably bed bound about 50% of my time. And if I was not in bed, I was seeking pain relief, usually in a hot bath. I would say within two weeks, the pain throughout my body had significantly subsided. I still had a little bit of joint pain but the overall soft muscle pain was GONE. I had been taking opioids for over a decade prior, and I practically eliminated all that. It was, it was pretty unbelievable. Pain was a huge factor. I wasn’t changing my doctors - but the one thing we all agreed on is that they found sudden improvement in me. In my gut, I was confident of the changes were from the use of PEMF.
I live a completely different life. To be clear, I'm not healed. I still have to live a more gentle life- certainly nothing like I used to do back in my army days or my early years working in corporate America- running and teaching aerobics and doing things like that. I still am not there to be able to do all that. The disease is still there, but the symptoms are managed and I have eliminated all the harsh, addictive medications. I am definitely getting so much more out of life without pain pills as opposed to being bed ridden and walking with a cane.
For anyone suffering like this, it's worth looking into. You want the expertise from the medical world, but you should blend the holistic treatments that are available- and then research it. If you search PEMF- read up on it! You'll find so many clinical studies and user testimonials that are coming up on that for all different ailments (not just mine) and they're seeing results.
Thanks to PEMF, I'm able to participate with my family. I'm able to travel, go to the beach and take wonderful walks again. My sisters and I started my own business helping horses and people (with PEMF) be more pain-free and traveling again. It's hard not to be passionate about something that has that effect on your life. My husband says he got his wife back.
SPECIAL THANKS
The editors of this spotlight proudly gives thanks to Ms. Suzanne Wheeler for her generosity in sharing her story and her resources with us. Additional thanks to Dr. Jerry Dreessen of the AOPP (Association of PEMF Professionals) and Pat Ziemer of Magnawave Inc. and Aura Wellness PEMF for coordinating our interviews, shared countless materials and conducted unending support to help our educational program bring new light to PEMF technology for chronic disorders and supportive testimonials in alternative therapeutics.
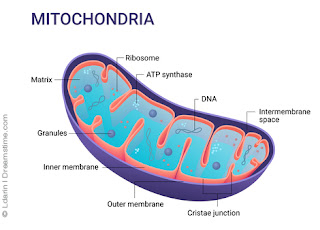
ScienceNews Extra Commentary on CFS/ME (Chronic Fatigue Syndrome and Myalgic Encephalomyelitis One of the key underlying findings in conditions causing chronic mental or physical fatigue is dysfunction of the mitochondria. Mitochondria are small structures located in the nucleus of every cell, and every cell contains thousands of them. These powerhouses produce the energy our bodies need to carry out every function in the form of ATP (adenosine triphosphate). When mitochondria don’t function at their best, or too many of them are destroyed, our energy levels suffer. While this can be due to inherited genetic disorders, most often it is seen as the result of chronic damage over time. Many of the biochemical reactions in our bodies produce toxic versions of oxygen, hydrogen and nitrogen, including how we make ATP. These toxic molecules, which we call free radicals, have to be neutralized so they don’t damage the mitochondria. Our bodies have powerful antioxidant defenses to keep these in check. But when these protective systems become overwhelmed by too many free radicals, oxidative stress results and mitochondria are damaged. |
IN THE NEWS
THE 2022 POST-MILITARY CRUSADERS COALITION2/11/2022- A 2022 initiative by community leaders launched the PMCC or Post Military Crusaders Coalition to launch an action plan for health resources for injured American veterans. Similar to the First Responders Cancer Resource project, this campaign supports all veteran advocates and service members support organizations by offering educational initiatives, alternative therapeutic modalities, sustainable diagnostic technologies and clinical research programs.